Connect With Us

Causes of Achilles Tendon Pain

Achilles tendonitis affects the Achilles tendon, which connects the calf muscles to the heel bone. Overuse or strain of the Achilles tendon can lead to inflammation and irritation, causing symptoms such as pain, tenderness, stiffness, and decreased strength and flexibility in the affected leg. This condition may develop gradually over time or suddenly during physical activity. In severe cases, Achilles tendonitis can progress to a partial or complete tear of the tendon. This results in more intense symptoms, like sharp pain, swelling, bruising, difficulty standing on tiptoe, or problems pointing the foot downward. Seeking prompt medical evaluation is important if you suspect Achilles tendonitis or experience symptoms of a tendon tear. Imaging tests, including ultrasound, X-rays, or MRI scans can confirm the diagnosis and determine the extent of the injury. If you are experiencing persistent symptoms of Achilles tendonitis, it is suggested that you make an appointment with a podiatrist for an exam, a diagnosis, and treatment options.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Lexington Foot and Ankle Center, PSC. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our offices located in Harrodsburg, Frankfort, Georgetown, and Lexington, KY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
What are Achilles Tendon Injuries
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
Risks Posed by Cracked Heels
 Leaving cracked heels untreated poses several risks that can affect your health. When the skin on the heels becomes excessively dry and develops calluses, it leads to deep fissures or cracks. These openings increase the risk of foot infections and leave an entry point for bacteria. Cracked heels can also lead to pain, discomfort, and difficulty walking, which may interfere with day-to-day activities. In severe cases, untreated cracked heels may result in bleeding and increase the risk of cellulitis, a serious bacterial skin infection. Foot wounds may develop when cracked heels become infected, and this is especially important to avoid for people with diabetes and the associated loss of circulation in the feet. Cracked heels may also signal underlying health issues, such as vitamin deficiencies or thyroid disorders. If you have cracked heels, it is suggested you make an appointment with a podiatrist who can treat the issue and prevent complications.
Leaving cracked heels untreated poses several risks that can affect your health. When the skin on the heels becomes excessively dry and develops calluses, it leads to deep fissures or cracks. These openings increase the risk of foot infections and leave an entry point for bacteria. Cracked heels can also lead to pain, discomfort, and difficulty walking, which may interfere with day-to-day activities. In severe cases, untreated cracked heels may result in bleeding and increase the risk of cellulitis, a serious bacterial skin infection. Foot wounds may develop when cracked heels become infected, and this is especially important to avoid for people with diabetes and the associated loss of circulation in the feet. Cracked heels may also signal underlying health issues, such as vitamin deficiencies or thyroid disorders. If you have cracked heels, it is suggested you make an appointment with a podiatrist who can treat the issue and prevent complications.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact one of our podiatrists from Lexington Foot and Ankle Center, PSC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our offices located in Harrodsburg, Frankfort, Georgetown, and Lexington, KY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
Pain in the Big Toe Joint

Pain in the big toe joint is a common source of discomfort that affects mobility and overall quality of life for many individuals. Whether stemming from age-related wear and tear, conditions like bunions, or physical injuries, understanding the underlying causes is vital for effective management. Hallux rigidus, characterized by joint degeneration and restricted movement, often accompanies osteoarthritis and may require surgical intervention in severe cases. Bunions are bony protrusions that often necessitate changes in footwear and orthotic support, with surgery as a potential solution for more severe cases. Physical injuries to the big toe joint can lead to swelling, pain, and an increased risk of developing arthritis or other joint-related issues. When conservative treatments fail to provide adequate relief, surgical options such as bunionectomy, joint realignment, or fusion may be needed. If you have persistent pain in the big toe, it is suggested that you make an appointment with a podiatrist for an exam and a diagnosis, before deciding on the right treatment.
Toe pain can disrupt your daily activities. If you have any concerns, contact one of our podiatrists of Lexington Foot and Ankle Center, PSC. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
- Trauma
- Sports injury
- Wearing shoes that are too tight
- Arthritis
- Gout
- Corns and calluses
- Hammertoe
- Bunions
- Blisters
- Ingrown toenails
- Sprains
- Fractures (broken bones)
- Dislocations
When to See a Podiatrist
- Severe pain
- Persistent pain that lasts more than a week
- Signs of infection
- Continued swelling
- Pain that prevents walking
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please feel free to contact our offices located in Harrodsburg, Frankfort, Georgetown, and Lexington, KY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Toe Pain
Toe pain can originate from corns, calluses, hammertoes, and bunions, as well as ingrown toenails, sprains, fractures, and dislocations. Corns develop as the toe rubs against the inside of a shoe which causes the skin to thicken as a form of protection. A corn is typically cone-shaped and has a small, hardened spot that points inward. When a corn is pressed into the skin, the toe becomes painful. Corns usually form on the top or side of the toe. A callus is also a thickened patch of skin that generally forms on the bottom of the foot. Calluses are the result of friction from the toe rubbing against the inside of a shoe. They may also occur by walking barefoot or having flat feet. A hammertoe is a bump on the knuckle of the second toe that is produced by wearing shoes that are too short for your feet. The bony protrusion rubs against the top of the shoe causing pain and irritation. A bunion is a malformation of the big toe. The base of the big toe pushes away from the smaller toes, forcing the top of the big toe to press toward the other toes. Bunions can be hereditary, or they can result from injury to the toe joint or from wearing high heels with a narrow toe box. The toe becomes inflamed, and a bump may develop at the end of the misplaced bone. Ingrown toenails typically affect the big toe and its surrounding skin. The nail will dig into the skin and become painful. Wearing tight or narrow shoes that compress the big toe causes the nail to grow into the fleshy part of the toe. Cutting toenails incorrectly can also add to the development of an ingrown toenail. A toe sprain originates from a torn or stretched ligament. Strapping the injured toe to the toe next to it for stabilization is common. A broken or fractured toe usually occurs from trauma like dropping a heavy object on it or bumping into something extremely hard and rigid. Osteoporosis, a thinning of the bones, can also bring about toe fractures.
Any of the conditions mentioned can lead to pain and irritation. While some are more serious than others, seeking an examination and diagnosis from a podiatrist is a good idea. A podiatrist can treat each ailment and get you back on your feet again without pain.
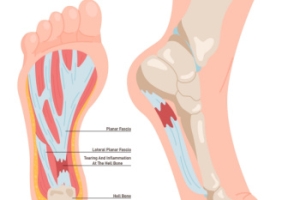
Key Insights Into Foot Pain From Plantar Fasciitis
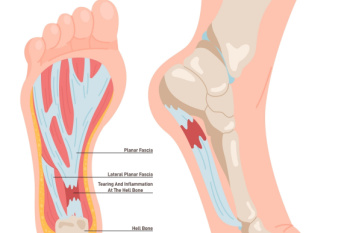
Plantar fasciitis, a common foot ailment, affects millions of individuals worldwide, causing discomfort and hindering mobility. This condition occurs when the plantar fascia, a thick band of tissue connecting the heel bone to the toes, becomes inflamed or strained. It is characterized by sharp pain at the bottom of the foot, particularly near the heel, especially noticeable during the first steps in the morning or after prolonged periods of rest. While the exact cause remains elusive, factors such as overuse, improper footwear, high-impact activities, and tight calf muscles contribute to its onset. Plantar fasciitis is prevalent among athletes, runners, and individuals who spend extended periods on their feet. Fortunately, conservative treatments like rest, stretching exercises, and orthotic inserts, can alleviate symptoms and promote healing in many cases. However, persistent cases may require medical intervention, including corticosteroid injections or surgical procedures. If you have heel pain, it is suggested that you confer with a podiatrist who can accurately diagnose and treat plantar fasciitis.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Lexington Foot and Ankle Center, PSC. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our offices located in Harrodsburg, Frankfort, Georgetown, and Lexington, KY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Many Causes of Foot Arch Pain

The human foot, with its intricate network of bones, is organized into two arches, one running the length of the foot and other the width. The arches are supported by ligaments, muscles, and the plantar fascia, which runs beneath the foot. They function as a shock absorbing system during walking. Foot pain can be felt in the arches, including muscle strain, ligament sprains, fractures, poor alignment, or tightness within the foot's structures. Inflammation of the plantar fascia, often due to injury or repetitive stress, commonly leads to discomfort and restricted mobility. Symptoms of arch pain can include a dull ache in the bottom of the foot, a sign of plantar fasciitis, or specific joint tenderness or swelling, which may indicate a sprain or fracture, necessitating prompt medical attention. Conditions such as arthritis or stress fractures can also result from repetitive stress or trauma to the foot muscles or bones. A physical examination by a podiatrist, imaging tests, and gait analysis may be needed. If you are suffering from arch pain, it is suggested that you schedule an appointment with a podiatrist for treatment options.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with one of our podiatrists from Lexington Foot and Ankle Center, PSC. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Harrodsburg, Frankfort, Georgetown, and Lexington, KY . We offer the newest diagnostic and treatment technologies for all your foot care needs.